Dr. Nenad Sestan, senior author of the new study and a professor of neuroscience, noted that blood flow and some energy use could be seen in the dead brains, but the neural circuits showed no higher-level function, including the global electrical activity needed for awareness.
Still, this new experimental system, called BrainEx (for ex vivo, or outside the body), may have “broader applications” — some relevant to humans, Sestan and his co-authors wrote: “This possibility raises important ethical considerations that must be addressed.”
“Could BrainEx ever be used with human brains? Is it possible in the future that more brain function could be restored?” wondered Christine Grady, chief of the Department of Bioethics at the National Institutes of Health Clinical Center. She added that these “logical questions” are not answered by the study, though it “raises them for consideration now and in the future as the science progresses.”
The research, which was funded by the National Institutes of Health’s BRAIN Initiative, was published Tuesday in the journal Nature.
Sophisticated artificial blood-pumping system
How can researchers study brain dynamics when, within minutes of death, the loss of blood flow causes irreversible damage in the brains of humans and other advanced mammals? To overcome this obstacle, Sestan and his colleagues created a system designed to lessen various processes of tissue degradation in postmortem brains.
Using brains from a pork processing plant, they applied the experimental BrainEx system, which pumps a blood-substitution fluid carrying nutrients and oxygen plus stabilizing compounds and activity blockers into each brain’s main arteries.
Stefano Daniele, co-author of the study and a member of Sestan’s lab, explained that after neurons are deprived of oxygen and blood flow, they “start to fire very rapidly, and this ironically leads to their own demise.” This activity, known as excitotoxicity, needs to be quelled to protect the neurons, and that’s why an activity blocker was necessary. In this case, the researchers used a sodium channel blocker commonly given to patients with seizure disorders.
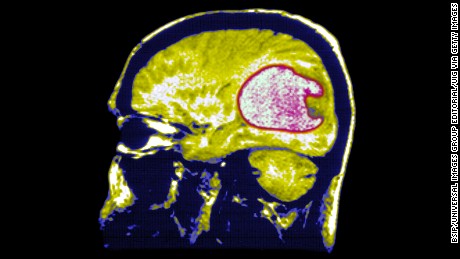
Next, they used ultrasound imaging, MRI and CT scanning to examine how cells were functioning and how blood flow and brain structure changed over time.
The brains flushed with this solution four hours after death showed reduced cell death; restored blood vessel structure and circulatory function; preserved anatomical and cell architecture, and restored some cellular inflammatory responses, spontaneous neural activity at synapses and active metabolism when compared with rapidly decomposing brains that were flushed with a solution lacking the same necessary ingredients.
Sestan emphasized that the research is still in the early stages. “This cannot be applied to humans at the moment. This is not a living, functioning brain”; it is only a “cellularly active brain.”
Going forward, his single goal is to discover whether this experiment can be done for a longer period using the “same paradigm, same pig brain, nothing else,” Sestan said. “Once we do this, we’ll see where we get.”
‘Surprising’ results
Andrea Beckel-Mitchener, team lead of the BRAIN Initiative at the National Institute of Mental Health, noted that the experiment “did not show resurgence or recovery of normal brain function; it was resiliency of brain tissue.” Still, she said, the result was surprising in that it was not known that “brain cells can maintain some healthy function hours after loss of blood flow.”
She describes BrainEx as “a real breakthrough” and anticipates experiments in which it is used as a tool for understanding basic biology underlying brain trauma and stroke, among other disorders, and to test how an experimental drug might affect the intricate 3D wiring of a large brain.
Grady noted that the experiment did not show resurgence of normal brain function. “Is there a place at which we would stop doing the research if we got too close to [resurgence of normal brain function]? I don’t think we’re too far away from that possibility at the moment to be able to say we would stop,” she said. “The ethically responsible course is to pursue the science to see where it will take us and what we can learn from it about brains.”
Martin Monti, an associate professor in the Departments of Psychology and Neurosurgery at University of California Los Angeles, told Science Media Centre that “the advance here is that, with the right technology, we might now have more time to recover some molecular, cellular, and microvascular function before these are completely compromised in the non-human animal model.”
This should not be confused with “acts of magic” restoring function in a favorite long-gone hero or “re-infusing cognitive processing or, much less, sentience in the decapitated head,” said Monti, who was not involved in the experiments. “For now, the cautious interpretation of this work is that, with this technology, the window for rescuing from the process of death profoundly damaged neural tissue, in the pig model, might be larger than we thought. Already a remarkable achievement.”
Derek Hill, a professor of medical imaging sciences at University College London, told Science Media Centre that “BrainEx most certainly didn’t bring the brains back to life — and in particular there was no evidence of any electrical nerve activity in the brain.”
However, Hill, who did not participate in the research, added that “this research raises some fascinating questions. Firstly, was this somehow a chance finding, or can it be reliably replicated? Secondly, could brains maintained by BrainEx help scientists discover new treatments for brain diseases like Alzheimer’s and Parkinson’s disease, which are proving really hard to treat? And thirdly, what are the ethical implications for the way we treat animals after slaughter, and humans after accidents.”
The authors of an editorial published alongside the new study wrote that “New guidelines are needed for studies involving the preservation or restoration of whole brains, because animals used for such research could end up in a grey area — not alive, but not completely dead.”
Grady noted that there are “clear rules about what you can do with humans. Once a human dies and their tissue is in a laboratory, there are many fewer restrictions on what could be done.” There may need to be “new rules,” she said.
Views: 287