The term psychosis refers to a range of symptoms which impact one’s thoughts, emotions, and behaviors, causing an individual to lose contact with reality. In recent years, psychotic disorders have become a hot topic of conversation within the cannabis community, sparking much debate.
A study published in March 2019 in Lancet Psychiatry found that those who consumed high-potency cannabis daily were three times more likely to have a psychotic episode compared with those who never used cannabis. High-potency was defined as cannabis containing more than 10 percent THC.
While there is a cause for concern here, media outlets are not discussing other possible contributing factors, as well as the complex bidirectional relationship that exists between cannabis use and psychosis.
Dr. Suzi Gage, a lecturer in psychology at the University of Liverpool in England, who researches the link between substance use and mental health told Weedmaps News, “This study is observational. It looks at what people choose to do, rather than randomizing people into different groups — as would be done in an experiment. Of course, in this case, it’s not possible to randomize based on cannabis use.”
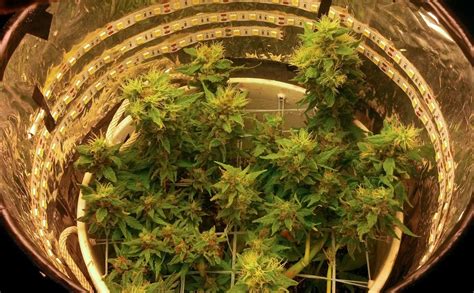
(Weedmaps file photo by Gina Coleman)
Gage, who also created the award-winning podcast, “Say Why to Drugs,” went on to explain, “People who choose to use cannabis every day are likely different from those who choose not to — in numerous ways other than just their cannabis use. As such, it’s challenging to rule out these differences.”
Cannabis May ‘Tip the Scales’
In recent years, cannabis use has been linked to an increased risk of psychosis. However, the available research is mixed and numerous confounding factors must still be considered.
“It might be that there are some people who have a pre-existing vulnerability, for example, a genetic predisposition to poor mental health, or other risk factors for psychosis, for example, childhood adversity, or any number of other risk factors,” Gage said. “For this group, heavy cannabis use could be one further factor that adds to their risk of developing psychosis. Psychosis is a complex disorder, and currently quite poorly understood.
“Heavy cannabis use might be one factor that tips the scales, but it’s not necessary or sufficient to cause psychosis, as we see from the many people who use cannabis and do not develop problems,” Gage added.
The most common disorder associated with symptoms of psychosis is schizophrenia, which has no single cause. According to one August 2018 study released by Radboud University in Nijmegen, Netherlands, that looked at data from 180,000 people, it appears that cannabis use and schizophrenia may share a genetic overlap. Overall, the researchers found 35 unique genes associated with cannabis use — and some of these genes are also associated with the risk of specific psychiatric conditions, including schizophrenia.
The researchers stated that this relationship may indicate a potential form of self-medication. Since substance use disorders are highly common among schizophrenia patients, occurring in up to 42 percent of patients, a possible dysfunction in the brain reward circuit is of key interest.
This isn’t surprising, as the biological and neurological mechanisms of cannabis overlap with those associated with schizophrenia, particularly in relation to the endocannabinoid system (ECS). For example, schizophrenia patients have a higher density of CB1 receptors in key areas of the brain.
There are also concerns surrounding the role of gene-environment selection, as researchers continue to study the impact of urban living in relation to the risk of schizophrenia.
Relationships Between Genetic and Environmental Variables
In terms of the potential mechanisms that may explain an increased risk of schizophrenia in relation to cannabis use, a person’s genetic makeup seems to play a very important role.
To understand the interaction between genes and cannabis exposure, researchers from Israel’s Sackler School of Medicine at Tel Aviv University gave THC to genetically modified mice which carry a gene that is common in people with schizophrenia. In normal mice, THC exposure during the animals’ adolescent phase didn’t impair their cognitive performance, but for the mice carrying the schizophrenia gene, THC caused a major loss of function. The researchers also tied this detrimental effect to deficits in a particular protein (BDNF), which preserves the brain’s homeostasis in the mice without the genetic mutation.
(Rafael Castillo/Flickr)
This means that psychotic disorders such as schizophrenia may at least partially be caused by an imbalance in the brain’s homeostasis, as triggered by the complex interaction between genetic and environmental variables. The above findings have clear implications for those who have a family history of psychosis. These individuals should be cautious when using cannabis, particularly during adolescence — not only in terms of psychosis risk, but also in relation to optimal development and addiction risk.
Who Is Most Vulnerable?
Although a stronger genetic predisposition to schizophrenia is more likely to influence lifetime cannabis use, a reverse cause-and-effect relationship cannot be excluded. This is particularly true in regards to factors such as the age at which cannabis is first used, the potency, frequency, and dosage.
Gage said, “All of the studies to date that have found a link between cannabis and psychosis have suggested that the risk for mental health issues comes from daily use of cannabis — particularly higher potency cannabis. I think a good way to think about this is to compare it to alcohol use. If a person was having a few beers per week, this is not a particularly worrying behavior pattern. However, if a person was drinking vodka every day, you might expect them to have a higher risk of negative consequences as a result of their behavior. The same could be true for cannabis.”
Correlation is not causation. Conclusive evidence is lacking in regards to definitive causation and now, the greatest priority is to understand who is most at risk and what other variables may be involved.
At this time, the consensus among researchers is that daily, high-potent cannabis use does increase the risk of psychosis. However, across the general population, the associated effect is small. Since cannabis use has a differential risk on those who are susceptible vs those who are not susceptible to psychiatric disorders, more research is required to better understand who is most vulnerable and why. Although we cannot ignore that this relationship exists, more research is needed to find a definitive link.
Featured Image: Photo by Alessandro Zambon via Unsplash